SAN DIEGO — Shortly after Jay Heydt got the COVID-19 vaccine, he signed up for a clinical trial to measure his immune response. He knew his odds of producing antibodies were low.
Heydt has leukemia. He’s one of the millions of Americans with a compromised immune system who may not be protected by vaccination.
“Unfortunately, I felt obligated to really kind of remain quarantined even after having the vaccine just as a precautionary measure,” he said.
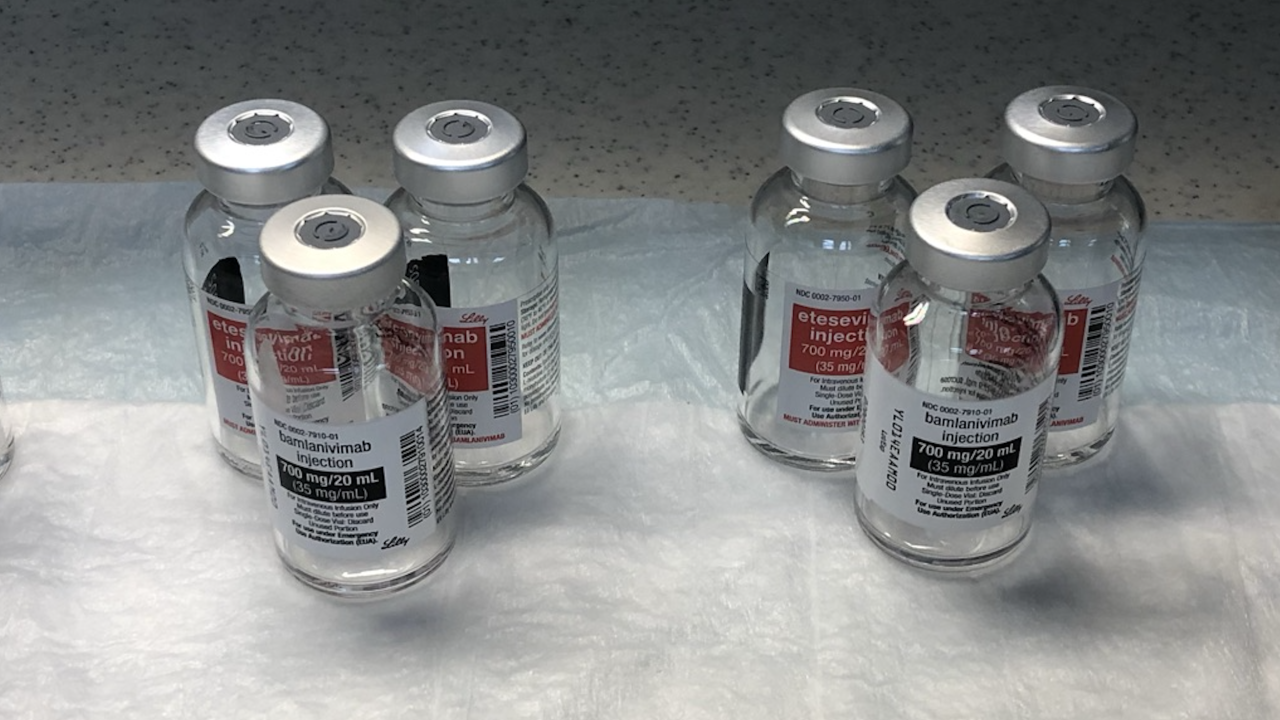
But scientists are now testing an alternative approach for patients who have trouble growing antibodies themselves: infusions of pre-made antibodies.
Lab-designed, cloned antibodies are already used to treat high-risk people after they get infected, but there are signs they can prevent infections too. A study published this month showed monoclonal antibodies made by Regeneron Pharmaceuticals were 81 percent effective at preventing infections in the first place.
Regeneron said April 12 that it would ask the Food and Drug Administration for authorization to use the antibody therapy as a preventative treatment.
“These antibodies may be particularly useful in individuals who are not yet vaccinated and may also have potential in those who are immunosuppressed and may not respond well to vaccines," said Dr. Dan H. Barouch, a Harvard Medical School professor who led the Regeneron trial.
Regeneron’s study was done on patients with normal immune systems, but the company is offering its therapy to immunocompromised patients under a compassionate use program, and other studies are underway. A monoclonal antibody by AstraZeneca that has been touted as a potential solution for immunocompromised people is now in Phase 3 trials.
There are about 10 million people considered immunocompromised in the U.S. It’s unclear how many of them may not respond to vaccination; experts believe it may depend on the type of their disease and the stage of their treatment.
Early research suggests the list of those who don't respond well includes organ transplant recipients and people with blood cancers. One small study released this month found 46 percent of the patients with blood cancers did not produce any antibodies after two doses with a COVID vaccine.
In February, the Leukemia and Lymphoma Society created a registry to recruit patients for clinical trials and distribute antibody tests to people with blood cancers.
Patients on certain medications also seem to have a weaker response. Those medications include Remicade for inflammatory bowel disease; Rituxan, which is used to treat certain cancers and autoimmune diseases like rheumatoid arthritis; and Gazyva or Imbruvica, which are treatments for certain blood cancers.
Those medications kill or block a type of white blood cell called B cells -- the cells responsible for making antibodies.
Dr. Thomas Buchholz, the medical director of Scripps MD Anderson Cancer Center and a Scripps Clinic physician, said that while pre-made antibodies are a promising theoretical solution for some patients, the approach is still unproven.
He said cancer patients should explore vaccination because the doses have been proven safe. Even though there are still unknowns about the level of protection in certain immunocompromised people, he said cancer patients can boost their chances of producing a strong immune response by coordinating vaccination into gaps between their chemotherapy and other treatments.
“Once you're vaccinated, you're going to have 24-7 availability of these innate cells that are alive and in your system,” he said. Vaccines also offer superior protection because they produce other immune cells beyond antibodies, like killer T cells and helper T cells.
Monoclonal antibodies, on the other hand, circulate for a while before fading out. “Eventually, they’re gone.”
To stay protected with monoclonal antibodies, patients may need infusions on a regular basis. Each one takes about 20 minutes.
Despite the inconvenience of regular infusions, patients like Jay Heydt say they’re curious about the potential treatment and are monitoring for news through the Leukemia and Lymphoma Society.
“I’m watching this very carefully,” he said.
And if monoclonal antibodies prove to offer better protection for people with compromised immune systems?
“I’m all in,” he said.
Derek Staahl at KGTV first reported this story.